Products You May Like
Exercise is good for you. That’s hardly news: People who exercise tend to have longer, healthier lives. But until recently, researchers have tallied its benefits only in narrow slices: Exercise lowers your cholesterol and blood pressure; it keeps you from getting fat. Now it’s becoming clear that those known slices don’t add up to the full pie.
“When people totaled up those effects, they only account for about half the benefit,” says Michael Joyner, an exercise physiologist at the Mayo Clinic in Rochester, Minnesota. “So what’s contributing to the biomedical dark matter?”
To solve that mystery, researchers are now digging deeper into the mechanisms that underlie the benefits of physical activity. They are finding that exercise is both powerful and wide-reaching, affecting not just muscles and the cardiovascular system, but almost every part of the body, from the immune system to the brain to the energy systems within individual cells. And as scientists understand more precisely which levers exercise pulls to improve our health, clinicians are on the verge of being able to change their practice. The goal is to think of exercise as a medicine—a therapy that they can prescribe in specific doses for specific needs.
“It’s like your own personal regenerative medicine,” says Joyner.
Brain Gains
Scientists have long known that some of the benefits of exercise are a simple matter of plumbing. Exercise makes blood vessels bigger and keeps them functioning smoothly, which makes them less likely to plug up and cause a heart attack or stroke. There have been hints that this may also mean more blood flow to the brain, which could help prevent cognitive decline. For example, studies have linked exercise to a reduced risk of Alzheimer’s.

Now researchers are making a more explicit connection between exercise and brain health. They are discovering that the full benefit of exercise comes not from mere physical movement but from actual physical fitness, the body’s cardiovascular health. A long-term study of Norwegian military recruits, for example, found that their aerobic fitness at age 18 was highly predictive of their risk of dementia in old age. And Swedish women who were highly fit in middle age had an eight times lower risk of dementia over the next 44 years than women of only moderate fitness, researchers reported in 2018 in Neurology.
Another recent study, led by K. Sreekumaran Nair, an endocrinologist at the Mayo Clinic, found that after just 12 weeks of a high-intensity exercise regimen, participants’ brains showed increased glucose uptake and higher metabolic activity, particularly in regions that usually show decline in Alzheimer’s disease. High-intensity exercise was found to have a similar effect on the parts of the brain most affected by Parkinson’s disease, in research led by Marcas Bamman, an exercise physiologist at the University of Alabama at Birmingham.
Benefits Of Brawn
Exercise doesn’t just build bigger blood vessels; it also builds bigger muscles. That benefits health in a number of ways, from minimizing the risk of diabetes to enhancing the body’s immune response to ills such as cancer.
Muscle is the largest consumer of all the glucose that floods into the bloodstream after a meal. More muscle means quicker removal of this glucose surge, says Bamman — and therefore, less exposure to the harm caused by elevated blood sugar, a serious health issue for people prone to diabetes.
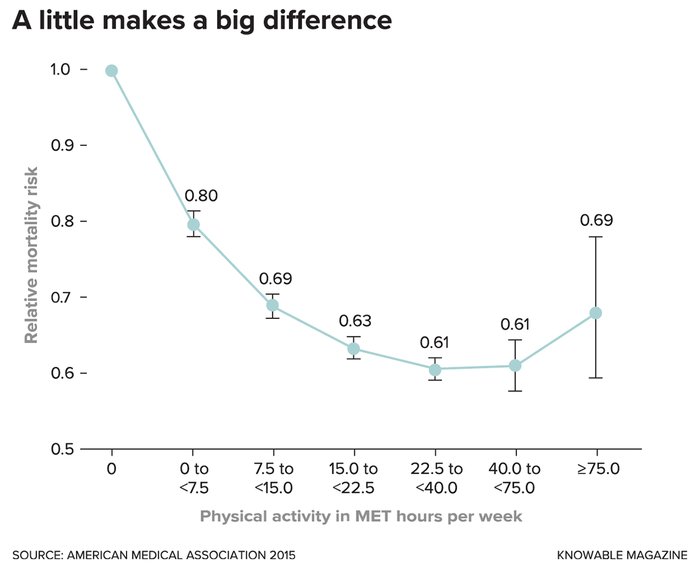
Just getting the minimum recommended amount of exercise (7.5 metabolic equivalent (MET) hours per week) reduces mortality risk by 20 percent compared with no exercise at all. Exercising a little more than that minimum continues to reduce the risk, but such benefits taper off after about three times the recommended minimum. (MET is the ratio of a person’s working metabolic rate relative to their resting metabolic rate, 1 MET is the rate of energy expenditure while at rest, walking at 3 to 4 miles-per-hour is considered to require 4 METs.)
The muscle-building aspects of exercise also help reverse a key change associated with aging: a decline in the function of mitochondria, our cells’ energy generators. This decline, often seen in sedentary individuals, can leave the mitochondria unable to completely burn the cellular fuel and that can lead cells to generate more oxidants, the oxygen-rich, reactive molecules that damage proteins and DNA.
Muscles are chock-full of mitochondria and exercise can help avoid this oxidative damage. Nair’s studies show that aerobic exercise, alone or in combination with strength training, improves people’s mitochondrial function, reduces the production of oxidants and forestalls oxidative damage. High-intensity aerobic exercise also encourages mitochondria to produce more of the proteins they use to burn fuel.
Muscle has another important role: Its abundant proteins serve as reservoirs of amino acids for the rest of the body. Usually, when other organ systems need amino acids, says Bamman, “those are drawn from muscle.” That’s especially important when someone is sick because the immune system needs lots of amino acids to make antibodies that fight infection.
The biggest benefit from building muscle, though, may come from the signaling molecules it pumps into the blood. Bente Klarlund Pedersen, an exercise physiologist at the University of Copenhagen, identified the most-studied of these signaling molecules back in 2000, and later coined a term for them: myokines. Since then, she and other researchers have found hundreds more, many of which are activated by exercise. These molecules, which are released in response to muscular exertion, help regulate muscle growth, nutrient metabolism, inflammation and a host of other processes. “I think for most people it’s difficult to understand why muscle work can influence my liver or be good for my brain or bones,” she says. Myokines serve as the link between muscle activity and these other organs.
One of the most important myokines in this crosstalk is interleukin-6. Released in response to muscular exertion, IL-6 has several effects, including suppressing hunger and enhancing the immune system’s response to cancer. Another signaling molecule, cathepsin B, triggers beneficial changes in the brain, including the production of new brain cells. Other signaling molecules can help moderate depression.
Inflammation Extirpation
Exercise, of course, also helps keep you thinner—and especially, it forestalls the accumulation of abdominal fat, a particularly harmful sort. One reason abdominal fat is so bad for you is its partnership with inflammation. “If we take out visceral fat and study it in the lab, we see that visceral fat is more inflamed than subcutaneous fat,” says Pedersen. “This inflammation will spill over into the blood, causing chronic systemic inflammation.”
Chronic inflammation, Pedersen suggests in the 2019 Annual Review of Physiology, may be the underlying reason why inactivity contributes to so many different diseases. “We know that being physically inactive increases the risk of approximately 35 different diseases or disorders,” she says. “And if you have one of these diseases—let’s say you have type 2 diabetes—you have increased risk of others, like cancer or heart disease. If we tie it all together, one feature of all these diseases is physical inactivity, and the other is chronic inflammation.”
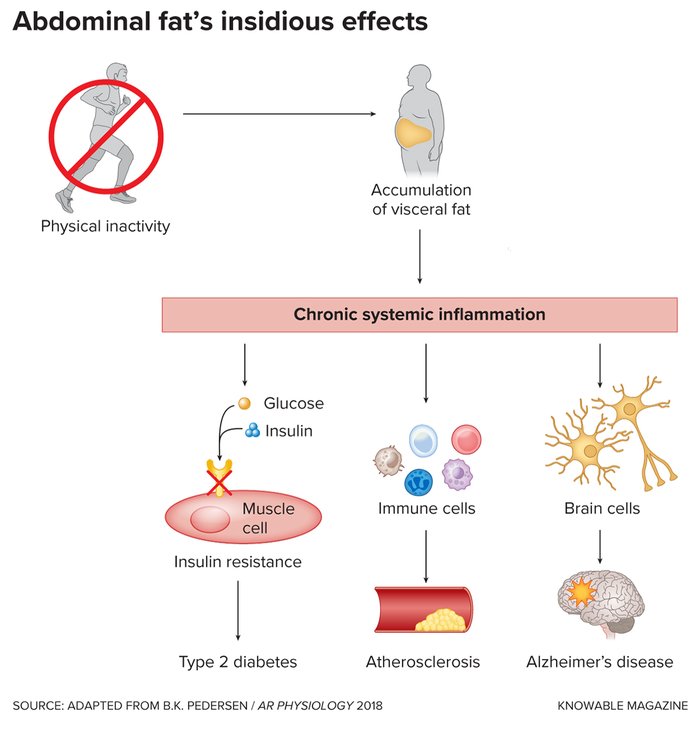
Even a few weeks of inactivity can cause fat to accumulate in the abdomen, which spurs chronic inflammation throughout the body. This inflammation contributes to a range of ailments, including type 2 diabetes, cardiovascular disease and Alzheimer’s disease.
About a decade ago, Pedersen conducted an experiment in which she had healthy young men reduce their daily step count from about 10,000 steps per day to just 1,500. Within two weeks, the men showed a 7 percent increase in abdominal fat mass. Along with this change, the men showed hints of reduced insulin sensitivity, a change also seen in type 2 diabetes.
Interleukin-6 appears to be at the heart of exercise’s effect on visceral fat and inflammation. In a recent experiment, Pedersen and her colleagues put 27 potbellied volunteers on a 12-week exercise-bike program, while 26 other volunteers remained inactive. Half the participants in each group also received a drug that blocks the action of IL-6. At the end of the 12 weeks, the exercisers had lost abdominal fat, as expected—but only if they had not received the IL-6 blocker. (Oddly, IL-6 is generally thought of as a pro-inflammatory molecule, because it is more abundant in obese people with systemic inflammation. But Pedersen has some evidence that in these people, elevated IL-6 is an effect, not a cause, of the inflammation.)
Rx For Movement
As researchers tease out more of the details about how physical activity benefits health, the moment is fast approaching when exercise becomes not merely “a good thing to do,” but a medicine in its own right, just like pharmaceutical drugs. Several studies already point in this direction. For example, more than half of 64 adults with type 2 diabetes were able to stop taking medication to lower their blood sugar within a year of beginning a regular exercise program, Pedersen and her team found. And a survey of more than 300 randomized controlled trials found that exercise was just as effective as drugs for people at risk of heart disease and diabetes, and was more effective than drugs for rehab after a stroke.
But if exercise is to truly become a medicine like any other, clinicians will need to learn how much to prescribe to maximize its benefits. “Just saying ‘be physically active’ is like telling people ‘eat better’—it doesn’t tell us what we should be doing,” says Kirk Erickson, an exercise psychologist at the University of Pittsburgh. But developing more precise dosing recommendations is difficult, because there are so many ways to exercise, which vary in duration, intensity, frequency and kind. (Tailoring to individual disease risks—telling one person to do X because they’re at risk of diabetes, and another person to do Y because of a family history of dementia—is an even more distant goal.)
Researchers are still working out what matters in this complex arena. Exercises that involve more muscle groups generate more IL-6, so full-body exercises like running have a greater anti-inflammatory effect than exercises that target just a few muscle groups, says Pedersen. And the benefits go away within a couple of days, suggesting that exercising frequently is important. “If it’s been 48 hours since you exercised, it’s time to do it again,” says Jill Barnes, an exercise physiologist at the University of Wisconsin-Madison.

A series of upcoming randomized trials may soon bring more certainty to the dosing question. One of the largest, which Bamman is involved with at the University of Alabama, will have nearly 2,000 volunteers undertaking either 12 weeks of endurance exercise, 12 weeks of weight training or no exercise program. Researchers will measure gene activity, molecular signaling and other changes within the body, which could allow them to pin down exactly how these two modes of exercise differ in effect. Because the study is so large, researchers should also be able to explore why some people respond more strongly than others to the same dose of exercise.
Another large study that Bamman is participating in, funded by the US Department of Defense, aims to compare genes activated by moderate exercise to those activated by high-intensity exercise in young, healthy volunteers.
Erickson is trying to parse the specifics with a study that will assess the effect of exercise volume on brain aging. Researchers will measure inflammation, signaling molecules, body composition and other markers, as well as mental acuity, on more than 600 volunteers ages 65 to 80, both before and after a year of exercise. Some of the volunteers will do 150 minutes per week of supervised moderate exercise, others will do 225 minutes per week, while a third group will do light stretching instead.
Of course, even after the results of these and other forthcoming trials are in, the “right” amount of exercise for a particular person is likely to depend on their individual circumstances. “For someone with diabetes who wants to improve blood-sugar control, even 10 minutes is probably great,” says Barnes. “But for cardiovascular risk or brain health, that may be different.”
Bamman agrees. “There’s not a single organ system in the body that isn’t affected by exercise,” he says. “Part of the reason the effect of exercise is so consistent and so robust is that there isn’t a single molecular pathway—it’s going to be a combination of all these things. So at the end of all these trials, we’re going to look back and list off not just one or two mechanisms, but a number of them. It’s going to be a complicated answer in the end.”
This article originally appeared in Knowable Magazine on Dec. 18, 2019. Knowable Magazine is an independent journalistic endeavor from Annual Reviews, a nonprofit publisher dedicated to synthesizing and integrating knowledge for the progress of science and the benefit of society. Sign up for Knowable Magazine’s newsletter.

